The potential problem lurking in psychedelic neuroscience.
Neuroscience's most popular tool for studying the psychedelic state may be fundamentally flawed.
We are living in a golden age of psychedelic neuroscience. The proverbial “psychedelic renaissance” has been well underway for over a decade at this point, and scientists are tackling the mysteries of the psychedelic state with tools that would have seemed like science fiction to psychologists in the 1950s. It seems like every week some new study drops showing a novel analysis of how drugs like LSD and psilocybin change brain activity, and as a neuroscientist interested in consciousness, I consider myself privileged to be alive and working in the field at this singular moment in scientific history. I’ve even been lucky enough to get to participate in the field myself, having published my own work on LSD, ketamine, and most recently, a little-known DMT analog called DPT. However, there is a big issue looming over the entire field, one that I have been worrying about for years, but which has gone resolutely un-discussed by pretty much everyone, even as the field marches on. This problem raises doubts about what is arguably the most popular brain imaging technology in use today: the functional MRI scan (fMRI), and how much we can actually learn from fMRI studies of psychedelic drugs. If my fears are correct, a huge amount of scientific work, done by scientists and theoreticians around the world might turn out to be fundamentally compromised.
This potential problem has nothing to do with consciousness, ego-death, spiritual experiences, or any of the other flashy features that make psychedelics so interesting to scientists and laypeople alike. Instead, it all goes back to the somewhat mundane fact that psychedelics raise your blood pressure by causing your blood vessels to contract. This effect is generally subtle enough that trippers won’t even notice it, but whether it’s in your skull, your legs, or your toes, taking a drug like LSD causes all of your blood vessels to tighten up. You’ll see it if you track your blood pressure before, during, and after a trip, though: a transient increase in pressure as the literal volume of space in your circulatory system contracts. This isn’t something unique to psychedelic drugs: almost any drug that tickles the serotonin system (and quite a few that don’t) have the same effect, known as vasoconstriction. Nevertheless, this could be a big problem for psychedelic scientists who build studies around comparing fMRI scans of the brain on psychedelics versus on a placebo.
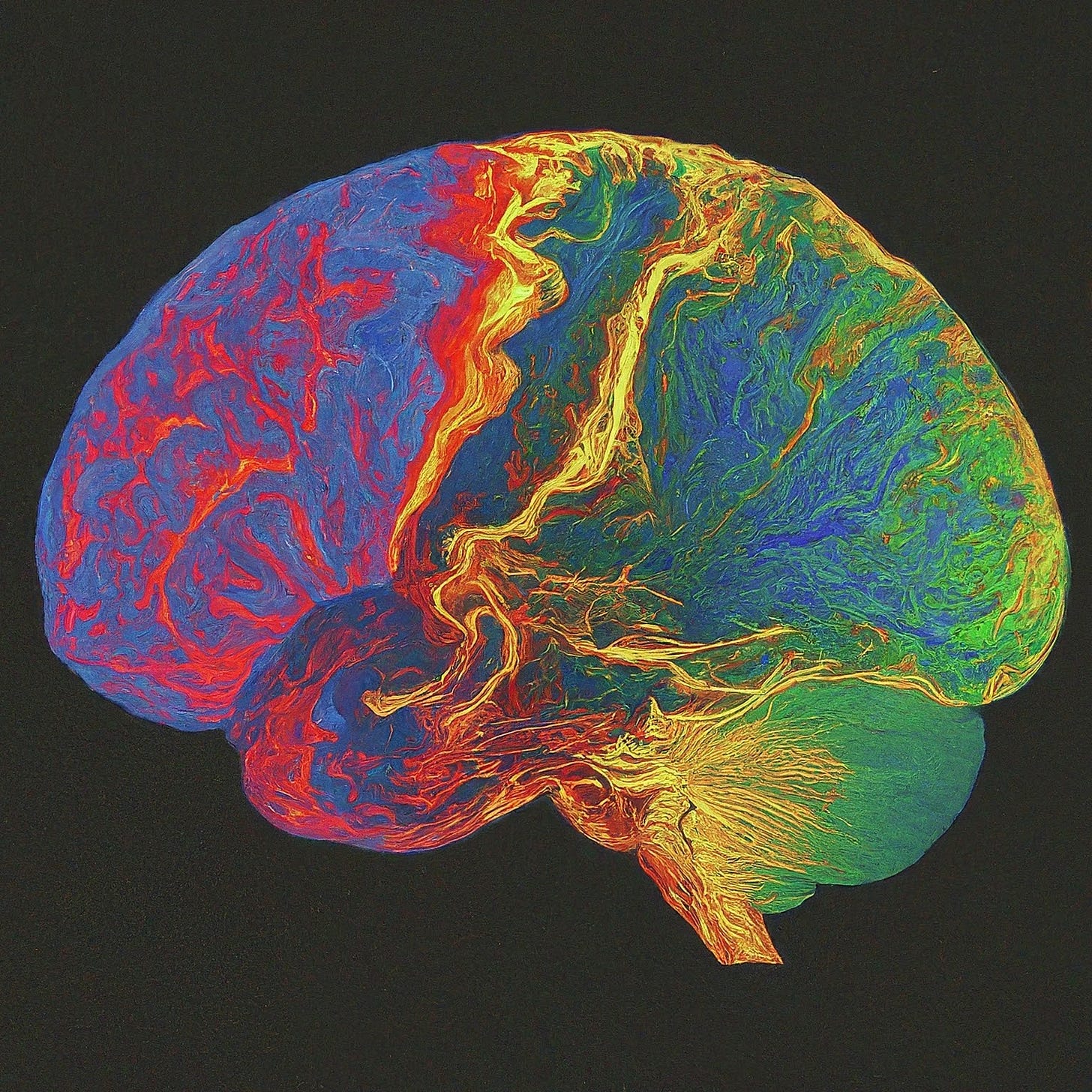
To understand why this is an issue, you unfortunately need to know a little bit about how fMRI works. The popular conception of fMRI is that it gives you a measure of how “active” a given area of the brain is: everyone has seen graphics in the popular press showing a brain, with different areas lit up like a Christmas tree. These brain regions, so the logic goes, are implicated in...whatever the brain (or mind) was doing during the scan.
This is not, strictly speaking true.
Or, if it is, it’s not the whole story. The signal you get out of an fMRI is not actually a direct measure of how active a given patch of cortex is. Instead, it’s a proxy measure, something called the BOLD signal, which stands for Blood Oxygen Level Dependent signal. You may already be seeing the issue from the name alone: the BOLD signal doesn’t really have anything directly to do with the brain – instead, it tracks the ratio of oxygenated hemoglobin to de-oxygenated hemoglobin in the blood flowing through the tissue. The idea is that, when neurons are active, they require increased supplies of oxygen to support the intense metabolic work of electrical signaling. This will lead to an increase in the amount of oxygenated blood flowing to those neurons, which can be read out on the BOLD signal. Note that the BOLD signal itself has nothing inherently to do with brain activity: you could conceivably use fMRI to explore oxygen dynamics in any part of the body, although in practice fMRI is almost entirely the provenance of computational and theoretical neuroscientists.
The question of whether changes in BOLD signal actually reflect meaningful changes in brain activity is a very well-studied one. By combining multiple modalities like fMRI + M/EEG, or doing invasive studies of living animal brains, it’s pretty clear that there is a link between BOLD activity and brain activity - it’s not a total wild goose chase. The link between brain activity and BOLD response is typically said to reflect neurovascular coupling, a fancy way of saying that there’s a connection between what the brain is doing and what the vascular system in and around the brain is doing. While it’s good to know that there’s a link between BOLD and brain activity (so neuroscience hasn’t completely wasted the last two decades of fMRI research), that link is also weak. If something were to change, or alter, the neurovascular coupling, then it would become much, much harder to interpret fMRI results.
This gets at a pretty fundamental assumption in fMRI research: the assumption that the underlying biology of the brain doesn’t change between conditions. If you’re comparing resting state (just lying in the scanner, not doing anything) with some kind of task (say, doing mental math), that assumption is probably fine. The brain doing mental math and the brain doing nothing may be running different “programs” (note the scare quotes), but the actual physical “hardware” (or “wetware”, maybe) doesn’t really change that much. It couldn’t, since we can bounce between resting state and mental math pretty seamlessly. When you enter the world of psychoactive drugs, however, this assumption pretty much goes out the window, but the field often just pretends that it doesn’t. Which brings us back to the problem of psychedelic neuroimaging.
Psychedelic drugs are powerful vasoconstrictors, a fact that has been known since the 1970s. This means that when you take a psychedelic drug, your blood vessels globally contract, becoming narrower and (incidentally) raising your blood pressure. There are a handful of cases of overdoses on psychedelics leading to “vasospasm”, or serious dysregulation of vascular tone – a phenomenon also typical of ergot poisoning. This vasoconstriction is global, which means that it also involves the blood vessels in the brain – the same blood vessels that are being monitored by the fMRI to estimate the BOLD signal. We can actually see the reduced blood flow to the brain caused by psychedelics in the clinic, using a related kind of neuroimaging called “arterial spin labeling”. Psilocybin reduces cerebral blood flow, and the degree of reduction correlates with intensity of experience.
Returning to the assumption that the “wetware” of the brain doesn’t change between conditions, it seems clear that, in the context of psychedelic fMRI, that assumption does not hold. Psychedelics are changing the flow of blood to the brain, and altering the dynamics of blood vessel expansion and contraction via vasoconstrictive activity. If the signal that you’re analyzing is based on cerebral blood flow, this is a truly massive confound, one that I think makes it very hard to be confident that we are interpreting fMRI studies correctly. As far as I can tell, this massive, glaring confound has gone almost entirely unaddressed in the scientific literature. Study after study after study is published showing how some fancy feature of BOLD signal dynamics are altered by psychedelics, but I have never seen anyone in the field stop and ask “are we sure that this actually reflecting a “software” difference, or is it an artifact of a “hardware” difference?” The closest I think we have come is some discussions I’ve seen on Twitter, and one opinion piece in The Conversation that came out recently and mentioned the vasoconstriction property as one of a litany of reasons to be cautiously skeptical about the hype around psychedelic neuroscience.
Honestly, this seems like a major failing of the field, and I confess that I myself have been part of it (part of my Masters degree research at Cambridge involved analyzing fMRI data from the famous Imperial LSD study). I don’t want to sound like I am attacking anyone (I consider many people in the field to be colleagues, mentors, and friends), but I also think it’s something that we have to take seriously. We can’t let the allure of pretty pictures and easy stories (that always go viral on social media and reliably generate citations) lead us down a garden path of cranking out material potentially built on a foundation made of sand.
I want to be clear, I cannot say for certain that the foundation is actually made of sand: it is entirely possible that none of this vasoconstriction stuff matters in the slightest for fMRI studies of psychedelics, and years from now people will say “wow, wasn’t Thomas Varley an anxious worrywort.” I don’t know.
But nobody else does either. And we’re not really talking about it, but instead just continuing to go full steam ahead.
The good news is that these questions are solvable, and pretty easily solvable at that. Someone needs to do an fMRI study looking at the effects of a cranial vasoconstrictor that doesn’t have mind-altering effects, and compare it to a psychedelic like psilocybin. Plenty of non-psychoactive vasoconstrictors are out there; in fact, since psychedelics induce vasoconstriction through their activity at serotonin receptors, many other serotonergic drugs have similar effects. One potentially useful class would be the triptan medications, which are prescribed as migraine abortives and even structurally resemble some psychedelics. I myself take rizatriptan for my chronic migraines and I can assure you that it is nothing like DMT (even though they are structurally quite similar).

How does the brain of someone tripping on a psychedelic look compared the brain of someone who just got a bolus of intravenous rizatriptan? I have no idea how they might be similar or different, but I would be intensely interested in finding out. We know that other, non-psychedelic vasoconstrictors (namely caffeine) can increase the entropy of BOLD activity in a way that is reminiscent of psychedelics, but we don’t know why or even what the underlying relationship between brain complexity and consciousness is. Is it possible that rizatriptan would induce similar effects? There’s only one way to find out.
Alternately, we could abandon fMRI for psychedelic neuroscience entirely, instead transitioning to modalities like EEG and MEG. I am sympathetic to this choice, as these approaches do not have the same limitations of fMRI and more directly measure activity in neural tissue rather than a proxy measure like BOLD. The fact that EEG is only a fraction of the cost helps, too. Of course, they also have a whole new set of limitations and problems – frankly, no neuroimaging technology in use today is as powerful as pop-neuroscience would have you believe – and any approach will require wrestling with complex trade-offs. I would say, however, that as things stand currently, that the issue looming over fMRI specifically is one that we shouldn’t ignore.
This may sound like a harsher critique of psychedelic science (and psychedelic scientists) than I mean it to. I do not think that anyone in the field right now is trying to put their thumbs on the scales or anything like that. However, in the last few weeks, we’ve gotten a look at what happens when psychedelic hype outstrips the technical requirements of doing really rigorous science: it comes back to bite us in the ass in a big way. As psychedelic neuroscience is only going to gain momentum in the coming years, it is imperative that we work out these boring, low-level technical problems first, before plowing headlong into the really fun stuff. And who knows, maybe the boring, low-level technical questions will prove to be a lot more interesting than we had initial believed.
Synergies is a reader supported publication.
If you don’t want to subscribe,
you can buy me a coffee instead, if you’d like..
Your support makes these articles possible.
Thank you for reading.



Good synopsis. There is also the issue of cardiac receptors for psilocin, etc. which are likely to cause changes in heart rate & HR variability at the same doses that produce neural effects. It's critical for fMRIers to account for all the physiological changes to attribute signals to neurovascular coupling. A good control drug might be the only effective way to do it since the mechanisms all overlap.
This post means so much to me. I have chronic headache post covid and am currently doing transcranial magnetic stimulation after doing an fmri. I'm 15 sessions in and was planning to recheck the fmri in ten or so sessions. I'm also debating other things uve discussed here.